What Triggers Heel Discomfort To Surface

Overview
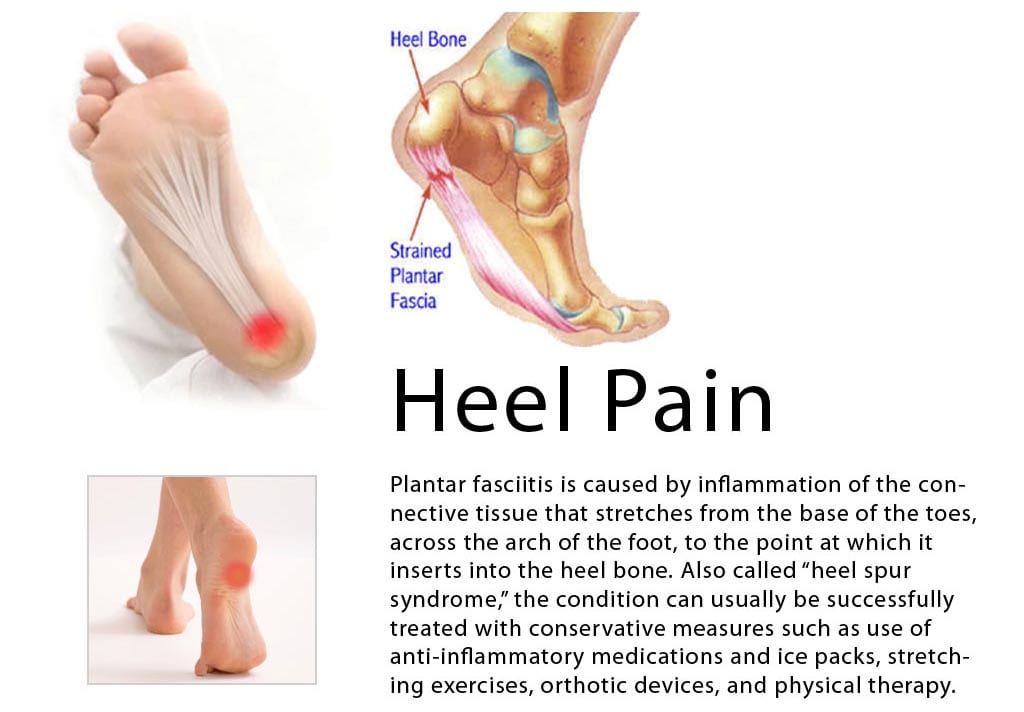
Plantar fasciitis is the most common cause of pain on the bottom of the heel. Approximately 2 million patients are treated for this condition every year. Plantar fasciitis occurs when the strong band of tissue that supports the arch of your foot becomes irritated and inflamed. The plantar fascia is a long, thin ligament that lies directly beneath the skin on the bottom of your foot. It connects the heel to the front of your foot, and supports the arch of your foot.
Causes
Plantar fasciitis symptoms are usually exacerbated via "traction" (or stretching) forces on the plantar fascia. In simple terms, you plantar fascia is repeatedly overstretched. The most common reason for the overstretching are an elongated arch due to either poor foot biomechanics (eg overpronation) or weakness of your foot arch muscles. Compression type plantar fascia injuries have a traumatic history. Landing on a sharp object that bruises your plantar fascia is your most likely truma. The location of plantar fasciitis pain will be further under your arch than under your heel, which is more likely to be a fat pad contusion if a single trauma caused your pain. The compression type plantar fasciitis can confused with a fat pad contusion that is often described as a "stone bruise".
Symptoms
The main symptom of plantar fasciitis is heel pain when you walk. You may also feel pain when you stand and possibly even when you are resting. This pain typically occurs first thing in the morning after you get out of bed, when your foot is placed flat on the floor. The pain occurs because you are stretching the plantar fascia. The pain usually lessens with more walking, but you may have it again after periods of rest. You may feel no pain when you are sleeping because the position of your feet during rest allows the fascia to shorten and relax.
Diagnosis
The health care provider will perform a physical exam. This may show tenderness on the bottom of your foot, flat feet or high arches, mild foot swelling or redness, stiffness or tightness of the arch in the bottom of your foot. X-rays may be taken to rule out other problems.
Non Surgical Treatment
Treatment for heel pain usually involves using a combination of techniques, such as stretches and painkillers, to relieve pain and speed up recovery. Most cases of heel pain get better within 12 months. Surgery may be recommended as a last resort if your symptoms don't improve after this time. Only 1 in 20 people with heel pain will need surgery. Whenever possible, rest the affected foot by not walking long distances and standing for long periods. However, you should regularly stretch your feet and calves using exercises such as those described below. Pain relief. Non-steroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, can be used to help relieve pain. Some people also find applying an ice pack to the affected heel for 5-10 minutes can help relieve pain and inflammation. However, do not apply an ice pack directly to your skin. Instead, wrap it in a towel. If you do not have an ice pack, you can use a packet of frozen vegetables.

Surgical Treatment
Surgery should be reserved for patients who have made every effort to fully participate in conservative treatments, but continue to have pain from plantar fasciitis. Patients should fit the following criteria. Symptoms for at least 9 months of treatment. Participation in daily treatments (exercises, stretches, etc.). If you fit these criteria, then surgery may be an option in the treatment of your plantar fasciitis. Unfortunately, surgery for treatment of plantar fasciitis is not as predictable as a surgeon might like. For example, surgeons can reliably predict that patients with severe knee arthritis will do well after knee replacement surgery about 95% of the time. Those are very good results. Unfortunately, the same is not true of patients with plantar fasciitis.
What Is Heel Pain And The Best Ways To Cure It
Overview
Plantar fasciitis is a condition that causes heel and arch pain through inflammation on the bottom of the foot. The part that’s inflamed (swollen) is actually the plantar fascia, which is the connective tissue or ligament that stretches from the base of the toes, across the arch of the foot, and inserts into the heel bone. This painful condition can interfere with your daily activity and severely decrease your quality of life.
Causes
Plantar Fasciitis often leads to heel pain, heel spurs, and/or arch pain. The excessive stretching of the plantar fascia that leads to the inflammation and discomfort can be caused by the following: Over-pronation (flat feet) which results in the arch collapsing upon weight bearing A foot with an unusually high arch A sudden increase in physical activity Excessive weight on the foot, usually attributed to obesity or pregnancy Improperly fitting footwear Over-pronation (flat feet) is the leading cause of plantar fasciitis. Over-pronation occurs in the walking process, when a person's arch collapses upon weight bearing, causing the plantar fascia to be stretched away from the heel bone. With Plantar Fasciitis, the bottom of your foot usually hurts near the inside of the foot where the heel and arch meet. The pain is often acute either first thing in the morning or after a long rest, because while resting the plantar fascia contracts back to its original shape. As the day progresses and the plantar fascia continues to be stretched, the pain often subsides.
Symptoms
The main symptom of plantar fasciitis is heel pain when you walk. You may also feel pain when you stand and possibly even when you are resting. This pain typically occurs first thing in the morning after you get out of bed, when your foot is placed flat on the floor. The pain occurs because you are stretching the plantar fascia. The pain usually lessens with more walking, but you may have it again after periods of rest. You may feel no pain when you are sleeping because the position of your feet during rest allows the fascia to shorten and relax.
Diagnosis
Most cases of plantar fasciitis are diagnosed by a health care provider who listens carefully to your description of symptoms. During an examination of your feet, your health care provider will have to press on the bottom of your feet, the area most likely to be painful in plantar fasciitis. Because the pain of plantar fasciitis has unique characteristics, pain upon rising, improvement after walking for several minutes, pain produced by pressure applied in a specific location on your foot but not with pressure in other areas, your health care provider will probably feel comfortable making the diagnosis based on your symptoms and a physical examination. Your health care provider may suggest that you have an X-ray of your foot to verify that there is no stress fracture causing your pain.
Non Surgical Treatment
Shoe therapy, finding and wearing shoes that allow your feet to be in their natural position, is the most important treatment for plantar fasciosis. Shoes that possess a flat heel, are wide in the toe box, lack toe spring, and have flexible soles are most appropriate for this foot problem. An increasing number of shoe companies are producing shoes with these design characteristics, but shoes that include all these features are still difficult to find. For some suggested footwear models, see our clinic’s shoe list. Most conventional footwear can be modified by stretching the shoe’s upper, stretching out the toe spring, removing the shoe’s liner, and cutting the shoe at certain key points to allow more room for your foot. Visit your podiatrist to help you with these shoe modifications. Correct Toes is another helpful conservative treatment method for plantar fasciosis. Correct Toes addresses the root cause of your plantar fasciosis by properly aligning your big toe and reducing the tension created by your abductor hallucis longus on the blood vessels that feed and "cleanse" the tissues of your plantar fascia. Your plantar fasciosis-related pain will diminish when the dead tissue is washed away. A rehabilitation program, which includes targeted stretches and other exercises, for your foot may be helpful too. Dietary changes and aerobic exercise are particularly important for overweight individuals who have plantar fasciosis. Water aerobics may be most appropriate for those individuals whose pain does not allow them to walk or cycle. Physical therapy may be another helpful treatment modality for this problem, and includes ultrasound, electrical stimulation, contrast baths, and range-of-motion exercises. Massage, acupuncture, reflexology, and magnet therapy are holistic approaches that may be helpful.

Surgical Treatment
Although most patients with plantar fasciitis respond to non-surgical treatment, a small percentage of patients may require surgery. If, after several months of non-surgical treatment, you continue to have heel pain, surgery will be considered. Your foot and ankle surgeon will discuss the surgical options with you and determine which approach would be most beneficial for you. No matter what kind of treatment you undergo for plantar fasciitis, the underlying causes that led to this condition may remain. Therefore, you will need to continue with preventive measures. Wearing supportive shoes, stretching, and using custom orthotic devices are the mainstay of long-term treatment for plantar fasciitis.
What May Cause Pain Under The Heel And How To Deal With It
Overview
Plantar fasciitis is the most common cause of pain on the bottom of the heel. Approximately 2 million patients are treated for this condition every year. Plantar fasciitis occurs when the strong band of tissue that supports the arch of your foot becomes irritated and inflamed. The plantar fascia is a long, thin ligament that lies directly beneath the skin on the bottom of your foot. It connects the heel to the front of your foot, and supports the arch of your foot.
Causes
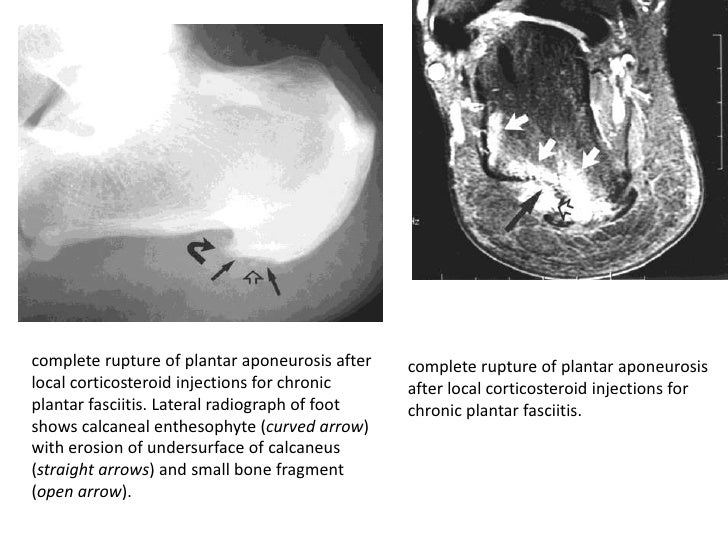
Training on improper, hard and/or irregular surfaces as well as excessive track work in spiked shoes, or steep hill running, can stress the plantar fascia past its limits of elasticity, leading to injury. Finally, failure in the early season to warm up gradually gives the athlete insufficient time for the structures of the foot to re-acclimate and return to a proper fitness level for intensive exercise. Such unprepared and repeated trauma causes microscopic tearing, which may only be detected once full-blown plantar fasciitis and accompanying pain and debilitation have resulted. If the level of damage to the plantar fascia is significant, an inflammatory reaction of the heel bone can produce spike-like projections of new bone, known as heel spurs. Indeed, plantar fasciitis has occasionally been refereed to as heel spur syndrome, though such spurs are not the cause of the initial pain but are instead a further symptom of the problem. While such spurs are sometimes painless, in other cases they cause pain or disability in the athlete, and surgical intervention to remove them may be required. A dull, intermittent pain in the heel is typical, sometimes progressing to a sharp, sustained discomfort. Commonly, pain is worse in the morning or after sitting, later decreasing as the patient begins walking, though standing or walking for long periods usually brings renewal of the pain.
Symptoms
The most common symptoms of plantar fasciitis include pain on the bottom of the foot near the heel, pain with the first few steps after getting out of bed in the morning, or after a long period of rest, such as after a long car ride. The pain subsides after a few minutes of walking. Greater pain after (not during) exercise or activity.
Diagnosis
After you describe your symptoms and discuss your concerns, your doctor will examine your foot. Your doctor will look for these signs. A high arch, an area of maximum tenderness on the bottom of your foot, just in front of your heel bone. Pain that gets worse when you flex your foot and the doctor pushes on the plantar fascia. The pain improves when you point your toes down. Limited "up" motion of your ankle. Your doctor may order imaging tests to help make sure your heel pain is caused by plantar fasciitis and not another problem. X-rays provide clear images of bones. They are useful in ruling out other causes of heel pain, such as fractures or arthritis. Heel spurs can be seen on an x-ray. Other imaging tests, such as magnetic resonance imaging (MRI) and ultrasound, are not routinely used to diagnose plantar fasciitis. They are rarely ordered. An MRI scan may be used if the heel pain is not relieved by initial treatment methods.
Non Surgical Treatment
The following recommendations are appropriate. Wear shoes with adequate arch support and cushioned heels; discard old running shoes and wear new ones; rotate work shoes daily. Avoid long periods of standing. Lose weight. Stretch the plantar fascia and warm up the lower extremity before participating in exercise. For increased flexibility, stretch the plantar fascia and the calf after exercise. Do not exercise on hard surfaces. Avoid walking barefooted on hard surfaces. Avoid high-impact sports that require a great deal of jumping (eg, aerobics and volleyball). Apply ice for 20 minutes after repetitive impact-loading activities and at the end of the day. Limit repetitive impact-loading activities such as running to every other day, and consider rest or cross-training for nonrunning days.

Surgical Treatment
When more conservative methods have failed to reduce plantar fasciitis pain, your doctor may suggest extracorporeal shock wave therapy, which is used to treat chronic plantar fasciitis. Extracorporeal shock wave therapy uses sound waves to stimulate healing, but may cause bruises, numbness, tingling, swelling, and pain. When all else fails, surgery may be recommended to detach the plantar fascia from the heel bone. Few people need surgery to treat the condition.
Prevention
Factors that help prevent plantar fasciitis and reduce the risk of recurrence include. Exercises to strengthen the muscles of the lower leg and ankle. Warming up before commencing physical activity. Maintaining a healthy body weight. Avoiding high heeled footwear. Using orthotic devices such as arch supports and heel raises in footwear, particularly for people with very high arches or flat feet. Daily stretches of plantar fascia and Achilles tendon.
What May Cause Heel Discomfort And The Way To Remedy It
Overview
Heel pain is most often caused by plantar fasciitis, a condition that is sometimes also called heel spur syndrome when a spur is present. Heel pain may also be due to other causes, such as a stress fracture, tendonitis, arthritis, nerve irritation, or, rarely, a cyst. Because there are several potential causes, it is important to have heel pain properly diagnosed. A foot and ankle surgeon is able to distinguish between all the possibilities and determine the underlying source of your heel pain. Plantar fasciitis is an inflammation of the band of tissue (the plantar fascia) that extends from the heel to the toes. In this condition, the fascia first becomes irritated and then inflamed, resulting in heel pain.
Causes
Patients with tight calf muscles will suffer with excessive pulling of the muscle group on the back of the heel. This in turn creates pulling of other structures that are attached to the heel, including the Plantar Fascia. When the pulling continues for long enough, then inflammation will develop and lead to Plantar Fasciitis. This causes Heel Pain. It is extremely common for patients who increase their level of activity to develop Plantar Fasciitis. Boot camp, running, zumba, recreational walking or other quick movement sports such as tennis or touch football are typical causes of Heel Pain. The sharp increase in exercise is too much for the foot to cope with and the stress on the Plantar Fascia causes inflammation. The Heel Pain that is caused by this inflammation is known as Plantar Fasciitis.
Symptoms
The main symptom of plantar fasciitis is heel pain when you walk. You may also feel pain when you stand and possibly even when you are resting. This pain typically occurs first thing in the morning after you get out of bed, when your foot is placed flat on the floor. The pain occurs because you are stretching the plantar fascia. The pain usually lessens with more walking, but you may have it again after periods of rest. You may feel no pain when you are sleeping because the position of your feet during rest allows the fascia to shorten and relax.
Diagnosis
Plantar fasciitis is one of many conditions causing "heel pain". Some other possible causes include nerve compression either in the foot or in the back, stress fracture of the calcaneus, and loss of the fatty tissue pad under the heel. Plantar fasciitis can be distinguished from these and other conditions based on a history and examination done by a physician. It should be noted that heel spurs are often inappropriately thought to be the sole cause of heel pain. In fact, heel spurs are common and are nothing more than the bone's response to traction or pulling-type forces from the plantar fascia and other muscles in the foot where they attach to the heel bone. They are commonly present in patients without pain, and frequently absent from those who have pain. It is the rare patient who has a truly enlarged and problematic spur requiring surgery.
Non Surgical Treatment
Plantar fasciitis can be a difficult problem to treat, with no panacea available. Fortunately, most patients with this condition eventually have satisfactory outcomes with nonsurgical treatment. Therefore, management of patient expectations minimizes frustration for both the patient and the provider.

Surgical Treatment
The majority of patients, about 90%, will respond to appropriate non-operative treatment measures over a period of 3-6 months. Surgery is a treatment option for patients with persistent symptoms, but is NOT recommended unless a patient has failed a minimum of 6-9 months of appropriate non-operative treatment. There are a number of reasons why surgery is not immediately entertained including. Non-operative treatment when performed appropriately has a high rate of success. Recovery from any foot surgery often takes longer than patients expect. Complications following this type of surgery can and DO occur! The surgery often does not fully address the underlying reason why the condition occurred therefore the surgery may not be completely effective. Prior to surgical intervention, it is important that the treating physician ensure that the correct diagnosis has been made. This seems self-evident, but there are other potential causes of heel pain. Surgical intervention may include extracorporeal shock wave therapy or endoscopic or open partial plantar fasciectomy.
Stretching Exercises
Stretching exercises for your foot are important. Do the stretches shown here at least twice a day. Don't bounce when you stretch. Plantar fascia stretch. To do the plantar fascia stretch, stand straight with your hands against a wall and your injured leg slightly behind your other leg. Keeping your heels flat on the floor, slowly bend both knees. You should feel the stretch in the lower part of your leg. Hold the stretch for 10 to 15 seconds. Repeat the stretch 6 to 8 times. Calf stretch. Stand with your hands against a wall and your injured leg behind your other leg. With your injured leg straight, your heel flat on the floor and your foot pointed straight ahead, lean slowly forward, bending the other leg. You should feel the stretch in the middle of your calf. Hold the stretch for 10 to 15 seconds. Repeat the stretch 6 to 8 times. Other exercises. You can also strengthen your leg muscles by standing on the ball of your foot at the edge of a step and raising up as high as possible on your toes. Relax between toe raises and let your heel fall a little lower than the edge of the step. It's also helpful to strengthen the foot by grabbing a towel with your toes as if you are going to pick up the towel with your foot. Repeat this exercise several times a day.
Symptoms Of Calcaneal Apophysitis
U-Shaped portion surrounds sore callus and reduces pain by transferring pressure from callus to the cushion. Soft orthotics cushion the ball and arches of the feet and protect them from injury and pain, while rigid orthotics correct abnormal foot angles and movements that can cause or worsen pain in the ball of the foot. Many insoles fit inside of slippers so that people suffering from pain in the ball of the foot can walk more comfortably inside their homes as well as outside. In addition, some insoles include added deodorizers to help decrease foot odor. While gel or foam insoles are sold at pharmacies, grocery stores and sporting-goods stores, orthotics require a visit to a podiatrist, who will make a cast of the foot and build a custom-fit insole from the cast. Foam, gel and soft orthotics require replacement once a year or more as the cushioning wears out. Rigid orthotics rarely need replacement. Hip bone spur can cause a lot of discomfort.
Most flat feet usually do not cause pain or other problems. Flat feet may be associated with pronation, a leaning inward of the ankle bones toward the center line. Foot pain, ankle pain or lower leg pain, especially in children, may be a result of flat feet and should be evaluated.

Do not consume food items which you are allergic to. Keep dead skin off your lips by lightly scrubbing them at least twice a week using a mild, natural ingredient such as cornflour or a lemon juice-sugar pack. I had a long road workout two weeks ago and immediately after starting having pain on the ball of my foot in this area. I have also learned buying shoes online is easy.
During the average lifetime our feet cover over 70,000 miles, the equivalent of walking four times around the world., so it's not surprising that problems can occur. Indeed around three-quarters of all adults will experience some sort of problem with their feet at some time. And without treatment most foot complaints will become gradually worse with time. This means people often endure painful conditions for far too long, and the problem can get worse. People often assume nothing can be done to help their condition, but in fact these conditions are extremely treatable. Swollen lump on big toe joint; lump may become numb but also make walking painful.
Chronic Back Pain Cure
Treatments can be made from drugs (such as anti-inflammatories, steroids, opiates and muscle relaxants), physical therapy and physical exercises, surgery or alternative treatments. Plants such as willow bark and arnica homeopathy and also are indicated. It is important that the patient always control your weight, maintain good posture, avoid smoking, get healthy lifestyles and practice sports. These measures help to treat and prevent the emergence of new pains. In some cases, back pain may radiate to other areas such as thighs and legs. In this situation, the most common cause is nerve compression that may be associated with disc herniation. Be certain you understand how to properly elevate objects. Lifting a heavy box might cause your back to scream at you in pain. There are many things to understand on the way to lift different objects. See the resources below for additional info on this. Use logic too. If it is too serious for you, get some assistance. You need to understand the seven Do's of lifting and bending within the resources below. A complete bed rest for 24 - 48 hrs relieves back pain in most of the instances. Walk a little every few hours to keep the blood flowing and the muscles toned. A cervical laminectomy (may be combined with an anterior approach) is sometimes performed when acute cervical disc herniation causes central cord syndrome or in cervical disc herniations refractory to conservative measures. Studies have shown that an anterior discectomy with fusion is the recommended procedure for central or anterolateral soft disc herniation, while a posterior laminotomy-foraminotomy may be considered when technical limitations for anterior access exist (e.g., short thick neck) or when the individual has had prior surgery at the same level (Windsor, 2006). The BlueCross BlueShield Association Technology Evaluation Center, the Washington State Health Technology Assessment Program, and the California Technology Assessment Forum are conducting reassessments of the vertebroplasty procedure. Various species of angelica have been used to quiet pain by American Indians throughout North America. The European species (Angelica archangelica) and the Chinese species (Angelica sinensis) have been used in the same way in the folk medicine of Europe and China respectively. The Chinese species is sometimes sold in North America under the names dang gui or dong quai. All species contain anti-inflammatory, antispasmodic, and anodyne (pain- relieving) properties. The European species of angelica has been used in European folk medicine since antiquity, as has the Chinese species in Chinese medicine. Low back pain is usually a signal of injuries or some underlying problem associated with the spine - its bones, muscles, and also other soft tissues. It could disrupt your job, regimen, and your activities. It may even impact your normal lifestyle as you are struggling to participate in recreational activities due to pain. If you would like fast-acting low back pain relief, you will find over the counter medicines obtainable in the majority of drugstores. These kinds of medicines can help to eliminate pain along with inflammation and offer back pain relief for patients. They consist of aspirin, acetaminophen (Tylenol), ketoprofen (Orudis), naproxen (Aleve), along with ibuprofen (Motrin). Studies have found that 20 to 25% of all chronic lower back pain comes not from the spine but from the sacroliac, or SI, joint, which bears and transfers weight and movement from your upper body to your legs. When the ligaments wear out and the SI joint becomes unstable, it can generate a similar kind of sharp back pain - or sciatica-like pain down your leg - as a ruptured disc. One study found that among "failed" spinal fusion patients - people who had their lumbar vertebrae fused and were still in pain afterward - the SI joint was the real culprit in more than half the cases. A thorough evaluation is useful in cases of prolonged discomfort or pain that reoccurs often. The first step may be an x-ray. It shows the bones of the spinal column and the status of the intervertebral discs can be evaluated indirectly. Computer tomography, MRI and neural pathway examination and EMG may be used as an additional diagnosis tools. In the most severe pain phase one can relax the back by lying on the back and lifting the legs against a wall or bending the knees on top of pillows. Follow the same rules with heat (15 minutes on, 1 hour off, repeat numerous times throughout the day) for best results. Lower back pain may result from a number of different causes, which may depend upon the individual's age. There are several things that you can do at home to relieve the pain, so you should explore all home treatment methods to determine the most effective one for you. Past research has hinted that low back pain, which affects roughly one in five people worldwide, could be related to the shape of the foot's arch in the standing position. Among 1,930 men and women recruited from Framingham, Massachusetts, pronated feet - which tend to roll inward as a person walks - were linked to lower back pain in women only.
Low back pain is usually a signal of injuries or some underlying problem associated with the spine - its bones, muscles, and also other soft tissues. It could disrupt your job, regimen, and your activities. It may even impact your normal lifestyle as you are struggling to participate in recreational activities due to pain. If you would like fast-acting low back pain relief, you will find over the counter medicines obtainable in the majority of drugstores. These kinds of medicines can help to eliminate pain along with inflammation and offer back pain relief for patients. They consist of aspirin, acetaminophen (Tylenol), ketoprofen (Orudis), naproxen (Aleve), along with ibuprofen (Motrin). Studies have found that 20 to 25% of all chronic lower back pain comes not from the spine but from the sacroliac, or SI, joint, which bears and transfers weight and movement from your upper body to your legs. When the ligaments wear out and the SI joint becomes unstable, it can generate a similar kind of sharp back pain - or sciatica-like pain down your leg - as a ruptured disc. One study found that among "failed" spinal fusion patients - people who had their lumbar vertebrae fused and were still in pain afterward - the SI joint was the real culprit in more than half the cases. A thorough evaluation is useful in cases of prolonged discomfort or pain that reoccurs often. The first step may be an x-ray. It shows the bones of the spinal column and the status of the intervertebral discs can be evaluated indirectly. Computer tomography, MRI and neural pathway examination and EMG may be used as an additional diagnosis tools. In the most severe pain phase one can relax the back by lying on the back and lifting the legs against a wall or bending the knees on top of pillows. Follow the same rules with heat (15 minutes on, 1 hour off, repeat numerous times throughout the day) for best results. Lower back pain may result from a number of different causes, which may depend upon the individual's age. There are several things that you can do at home to relieve the pain, so you should explore all home treatment methods to determine the most effective one for you. Past research has hinted that low back pain, which affects roughly one in five people worldwide, could be related to the shape of the foot's arch in the standing position. Among 1,930 men and women recruited from Framingham, Massachusetts, pronated feet - which tend to roll inward as a person walks - were linked to lower back pain in women only.
Foot Corn Prevention
It's better to cut your toenails after you do the soaking and lotion steps because the toenails are pretty thick and it's much easier when they are softened. Use a toenail clipper with a straigt edge so you don't cut them too short. Cutting your toenails too short can cause ingrown toenails and they are not fun! Next file your nails with the emery board. Create a relaxing spa treatment at home, put your feet your hands (or), a stone massage with natural essential oils. Feel free to use the oil in your closet, if available read more People suffering from Metatarsalgia often experience a burning sensation under the ball of the foot. Sometimes combined with a sharp, tingling sensation near the toes (this condition is called Morton's Neuroma, see further below). The pain can also be stabbing pain that comes and goes throughout the day. In some cases people experience a feeling similar to having a pebble sitting under the forefoot. Ball of Foot pain worsens when wearing high heels/fashion shoes for a longer periods of time or, for men after walking long distances in hard shoes. Typically people with Ball of Foot pain also display excessive callous formation under the balls of their feet. Three times a week, after you get out of the shower before you put on your socks or nylons or before you get into bed apply a cream or lotion containing 2% salicylic acid (BHA—beta hydroxy acid). On the days or nights when you don’t apply a BHA product apply an emollient, thick moisturizer such as pure shea butter or cocoa butter that you can buy at most drugstores or health food stores. Apply the paste to the callus. Place your foot or hand in a plastic bag and wrap a damp towel around it. Leave the paste on the callus for 15 minutes. You Might Also Like Step 4 So if you have rough dry heels and calluses on your feet, if your hands are rough from dishwashing, if your knees and elbows are rough and dry, I highly recommend this product. It is inexpensive, it works, it smells great and it does not have a greasy feel and the tube looks like a foot at the end and it has a snap close cap unlike many other creams. Nobody wants to have to put a cap on a tube when your hands are coated with the product. So they have just about covered everything to make the usage easier. A corn, or heloma, is a thickened area of dry skin that has a visible centre, or nucleus, at the area of greatest pressure. It is caused by direct pressure from shoes upon a bony surface of the foot. The centre, or nucleus, presses on nerve endings in the skin. If it is large enough, it can be quite painful. If the corns and calluses have been caused by repetitive actions, avoiding them will most probably solve the problem. Wearing shoes and socks that fit properly, as well as having protective pads and other self-care measure also help. However, when diabetes and peripheral neuropathy enter the picture, there is increasing evidence that excessive callusing may indeed be harmful to foot health. A callus may hide and even worsen inflammation that occurs under the callus The inflammation may be an early sign of a diabetic foot ulcer. Perhaps most concerning is that inflammation under calluses may be very hard to detect. In the Nishide study, experienced wound care nurses and specialists could not identify the latent inflammation in the calluses, even though three of the five inflamed calluses had tissue damage reaching down to the muscle layer. Several factors usually combine to cause rough, callous feet. Dry weather, bad footwear choices and repetitive foot motions can all cause your feet to become thick and callous-especially unfortunate when you want to wear foot-baring shoes, calluses are meant to protect your feet, but look ugly. Smooth out feet by exfoliating the skin and applying nourishing moisturizers to get the soft, touchable feet you want to show off in sandals and open-toed shoes. Step 1 You can usually keep the same wrap on your feet for up to two or three days before it needs changed. Be sure to consult a professional before attempting any self treatment for foot problems. Six percent of the United States population suffers with fallen archesor flat feet, according to the Illinois Podiatric Medical Association. Doctorprescribed exercises, physical therapy and the right kind of shoes helps flatfeet sufferers regain some shape to their feet. Of the remaining 94 percentthat have slight arches to high arches, the need for exercise is equallyimportant. With the help of some household items, you can train and exerciseyour feet and your arches without spending money for equipment or classes atthe gym. Combine lightly mashed strawberries with olive oil and salt. Don't over blend or mixture will become runny. Rub over feet to smooth rough calluses and rinse.
A corn, or heloma, is a thickened area of dry skin that has a visible centre, or nucleus, at the area of greatest pressure. It is caused by direct pressure from shoes upon a bony surface of the foot. The centre, or nucleus, presses on nerve endings in the skin. If it is large enough, it can be quite painful. If the corns and calluses have been caused by repetitive actions, avoiding them will most probably solve the problem. Wearing shoes and socks that fit properly, as well as having protective pads and other self-care measure also help. However, when diabetes and peripheral neuropathy enter the picture, there is increasing evidence that excessive callusing may indeed be harmful to foot health. A callus may hide and even worsen inflammation that occurs under the callus The inflammation may be an early sign of a diabetic foot ulcer. Perhaps most concerning is that inflammation under calluses may be very hard to detect. In the Nishide study, experienced wound care nurses and specialists could not identify the latent inflammation in the calluses, even though three of the five inflamed calluses had tissue damage reaching down to the muscle layer. Several factors usually combine to cause rough, callous feet. Dry weather, bad footwear choices and repetitive foot motions can all cause your feet to become thick and callous-especially unfortunate when you want to wear foot-baring shoes, calluses are meant to protect your feet, but look ugly. Smooth out feet by exfoliating the skin and applying nourishing moisturizers to get the soft, touchable feet you want to show off in sandals and open-toed shoes. Step 1 You can usually keep the same wrap on your feet for up to two or three days before it needs changed. Be sure to consult a professional before attempting any self treatment for foot problems. Six percent of the United States population suffers with fallen archesor flat feet, according to the Illinois Podiatric Medical Association. Doctorprescribed exercises, physical therapy and the right kind of shoes helps flatfeet sufferers regain some shape to their feet. Of the remaining 94 percentthat have slight arches to high arches, the need for exercise is equallyimportant. With the help of some household items, you can train and exerciseyour feet and your arches without spending money for equipment or classes atthe gym. Combine lightly mashed strawberries with olive oil and salt. Don't over blend or mixture will become runny. Rub over feet to smooth rough calluses and rinse.